What is endometriosis?
Endometriosis is a condition where tissue similar to the womb’s inner lining (endometrium) is found elsewhere, usually in the pelvis around the womb ovaries and fallopian tubes. It is a prevalent condition, affecting around 1 in 10 women. You are more likely to develop endometriosis if your mother or sister has had it. Endometriosis usually affects women during their reproductive years. It can be a long-term condition that can significantly impact your general physical health, emotional well-being and daily routine.
What are the symptoms of endometriosis?
Common symptoms include pelvic pain and painful, sometimes irregular or heavy periods. It can cause pain during or after sex and can lead to fertility problems. You may also have pain related to your bowels, bladder, lower back or the tops of your legs, and experience long-term fatigue. Some women with endometriosis do not have any symptoms. Endometriosis can cause pain that occurs in a regular pattern, becoming worse before and during your period. Some women experience pain all the time but for others, it may come and go. The pain may get better during pregnancy and sometimes it may disappear without any treatment.
What causes endometriosis?
The exact cause of endometriosis is not known but it is hormone dependent. This means that, just like the endometrium which responds to hormonal changes resulting in a period, the endometrial-like tissue located outside the womb also bleeds. This bleeding can cause pain, inflammation and scarring, and can possibly damage your pelvic organs.
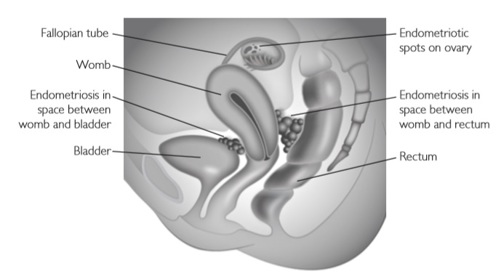
Endometriosis may be found:
- on the ovaries, where it can form cysts (often referred to as endometriomas or ‘chocolate cysts’)
- in the peritoneum (the lining of the pelvis and abdomen)
- in or on the fallopian tubes
- on, behind or around the womb
- in the area between the vagina and the rectum.
Endometriosis can also occur within the muscle wall of the womb (adenomyosis) and occasionally on the bowel and/or bladder. It may sometimes be found in other parts of the body, but this is rare.
How is it diagnosed?
A discussion about your symptoms and a physical examination should provide your doctor with enough information to determine if you might have endometriosis. Endometriosis can be a difficult condition to diagnose. This is because:
- the symptoms of endometriosis vary so much.
- the symptoms are common and can be similar to pain caused by other conditions such as irritable bowel syndrome (IBS) or pelvic inflammatory disease (PID).
- different women have different symptoms.
- some women have no symptoms.
What tests might I be offered?
Tests usually include:
- A pelvic ultrasound scan. This may be a transvaginal scan to check the uterus and ovaries. It may show whether there is an endometriotic (also known as a ‘chocolate’) cyst in the ovaries or may suggest endometriosis between the vagina and rectum.
- You may be offered a laparoscopy, which is the only way to get a definite diagnosis. This is carried out under a general anaesthetic. Small cuts are made in your abdomen and a telescope is inserted to look at your pelvis. You may have a biopsy to confirm the diagnosis and images may be taken for your medical records. Your Gynaecologist may suggest treating the endometriosis at the time of your first laparoscopy, either by removing cysts on the ovaries or treating any areas on the lining of your pelvis. This may avoid a second operation. Sometimes, however, the extent of endometriosis found means that you may need further tests or treatment.
What are my options for treatment?
When pain is the main problem, the treatment aims to relieve symptoms and lessen the pain.
- Simple pain relievers (paracetamol, etc): Many women will experience some relief of symptoms with over-the-counter medications such as paracetamol (Panadol) and non-steroidal anti-inflammatories (Ponstan, Nurofen, Naprogesic, etc).
- Hormonal treatments (the Pill, etc): Hormone treatments are used to suppress the normal menstrual cycle, which in turn stops or slows endometriosis growth and in some women are effective in reducing endometriosis-related pain. Hormonal treatments are available in multiple types, including tablets (such as the combined oral contraceptive pill – ‘the pill’), intrauterine devices (the Mirena), implants or injections.
- Laparoscopy (keyhole surgery): Surgery may assist in the diagnosis of endometriosis, especially for minimal or mild endometriosis where ultrasound scans may be normal. Surgical treatment often improves pain symptoms associated with endometriosis and is offered in addition to hormonal treatments.
- Hysterectomy: In a small group of women who have severe symptoms that are not relieved by medical or other surgical treatment, more extensive surgery such as hysterectomy (removal of the uterus, cervix and fallopian tubes) with or without removal of the ovaries may be considered.
- Bowel surgery: Sometimes endometriosis affects the wall of the bowel. When this is causing significant symptoms it may be suggested that the affected piece of bowel is removed. This surgery is performed in conjunction with a specialist colorectal (bowel) surgeon.



